The Labeling 2-2 Reference Manual serves as a comprehensive guide for accurate specimen labeling in healthcare settings. It provides standardized procedures for blood, urine, and tissue samples, ensuring consistency and patient safety.
Purpose and Scope of the Manual
The Labeling 2-2 Reference Manual is designed to provide clear, standardized instructions for accurately labeling biological specimens in healthcare settings. Its primary purpose is to ensure consistency and patient safety by outlining specific guidelines for blood, urine, and tissue samples. The manual covers the essential steps for proper labeling, including specimen collection, handling, and storage. It also addresses common errors and their implications, offering practical solutions to mitigate risks. The scope extends to various laboratory tests, ensuring that each labeled specimen meets the required standards for accurate analysis. By adhering to the manual’s protocols, healthcare professionals can minimize errors and improve overall efficiency in laboratory processes. This resource is invaluable for maintaining high standards of specimen labeling across diverse healthcare environments.
Key Components of the Labeling Exercise
The Labeling 2-2 Reference Manual emphasizes the importance of accurate specimen identification through clear guidelines. Key components include proper use of patient identifiers, such as name and date of birth, and specimen type designation. The manual outlines specific requirements for blood, urine, and tissue samples, including recommended aliquot volumes and storage conditions. It also details labeling formats, such as font size and barcode usage, to ensure readability and compatibility with laboratory systems. Additionally, the manual addresses error prevention strategies, like double-checking labels before submission, to minimize risks of misidentification. These components collectively ensure that labeled specimens meet standardized criteria for accurate and reliable laboratory testing, maintaining patient safety and data integrity throughout the process.
Understanding the Labeling Process
The labeling process involves collecting, preparing, and accurately marking specimens with patient identifiers and test details. It ensures traceability and safety, adhering to standardized protocols for reliable results.
Importance of Accurate Labeling in Healthcare
Accurate labeling is crucial in healthcare to ensure patient safety and reliable test outcomes. Mislabeling can lead to diagnostic errors, inappropriate treatments, and legal issues. Proper labeling ensures specimens are correctly matched to patients, reducing mix-ups and delays. It also maintains the integrity of laboratory processes, preventing false results that could endanger lives. Additionally, accurate labeling facilitates efficient tracking and communication among healthcare providers, contributing to better patient care. Adhering to standardized labeling protocols minimizes errors and ensures compliance with regulatory requirements, safeguarding both patients and healthcare institutions from potential risks. This underscores the necessity of meticulous attention to detail in specimen labeling.
Common Labeling Errors and Their Implications
Common labeling errors include illegible handwriting, incomplete patient information, and mismatched specimen containers. These mistakes can lead to severe consequences, such as delayed or incorrect diagnoses. Illegible labels may result in specimen rejection, requiring re-collection, which causes patient inconvenience. Incomplete information can lead to specimen mix-ups, potentially endangering patient lives. Mismatched containers and labels can cause cross-contamination or misidentification, affecting test accuracy. Such errors can also lead to legal and financial repercussions for healthcare institutions. Addressing these issues requires rigorous training, use of automated labeling systems, and adherence to strict protocols to minimize risks and ensure patient safety. Proper error detection and correction mechanisms are essential to mitigate these challenges effectively.
Labeling 2-2 Reference Manual: An Overview
The Labeling 2-2 Reference Manual provides standardized procedures and guidelines for accurate specimen labeling, ensuring consistency, safety, and compliance in healthcare settings.
The Labeling 2-2 Reference Manual is designed to provide clear, concise instructions for labeling biological specimens. Its primary purpose is to ensure accuracy and consistency in healthcare settings. The manual covers various specimen types, including blood, urine, and tissue samples, each with unique labeling requirements. By adhering to the guidelines outlined, healthcare professionals can minimize errors and enhance patient safety. The scope extends to both routine and specialized testing, offering detailed protocols for proper specimen identification and handling. This ensures that all laboratory tests are conducted efficiently and reliably, maintaining the highest standards of quality and patient care.
The Labeling 2-2 Reference Manual emphasizes several key components essential for accurate specimen labeling. First, it highlights the importance of using standardized labels, ensuring clarity and readability. Second, it outlines specific specimen collection requirements, such as volume and container type, to prevent processing delays. Third, the manual provides detailed instructions for labeling different types of samples, including blood, urine, and tissue, each with unique considerations. Additionally, it addresses error prevention strategies, such as double-checking patient identifiers and using barcode scanning. These components collectively ensure that specimens are correctly identified and processed, maintaining the integrity of laboratory results and patient safety. Adherence to these guidelines is crucial for effective specimen management in healthcare settings.
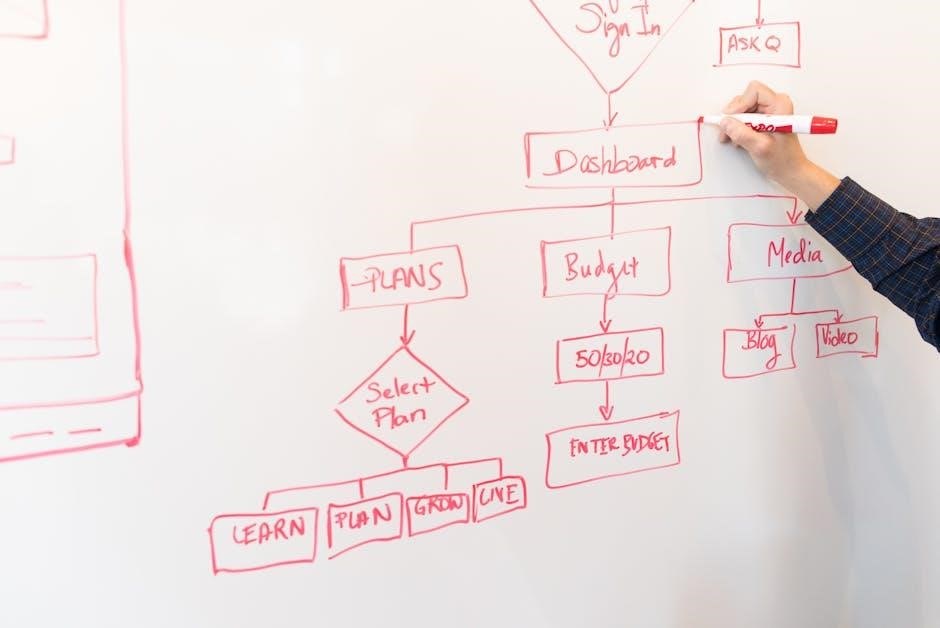
How to Use the Manual Effectively
To use the Labeling 2-2 Reference Manual effectively, begin by familiarizing yourself with its structure and content. Start with the table of contents to locate relevant sections quickly. Always follow the step-by-step guidelines for labeling blood, urine, and tissue samples, paying close attention to specific requirements like specimen volume and container type. Verify patient identifiers and use barcode scanning to minimize errors. Refer to the troubleshooting section for resolving common labeling issues, such as illegible labels or missing information. Regular practice and adherence to the manual’s protocols will enhance your proficiency. Stay updated with any revisions to ensure compliance with current standards. Consistent use of the manual guarantees accurate and reliable labeling, critical for patient safety and laboratory accuracy.
Practical Applications of the Manual
The manual provides standardized procedures for labeling blood, urine, and tissue samples, ensuring consistency and accuracy in healthcare settings. It aids in minimizing errors and improving patient safety.
Labeling Blood Samples: Guidelines and Best Practices
Accurate labeling of blood samples is critical for patient safety and reliable test results. The manual emphasizes using permanent markers, avoiding abbreviations, and ensuring all labels are legible. Each sample must include the patient’s name, date and time of collection, and the test requisition number. Special handling instructions, such as temperature requirements, should also be noted. Labeling errors can lead to delayed or incorrect treatment, making adherence to these guidelines essential. Best practices include double-checking labels before sending samples to the lab. These procedures help maintain the integrity of blood samples and support accurate diagnostic outcomes, ensuring efficient and effective healthcare delivery. Proper labeling is a cornerstone of quality patient care.
Labeling Urine Samples: Specific Requirements
Labeling urine samples requires precise adherence to guidelines to ensure accurate test results. The manual specifies that each sample must be labeled with the patient’s name, date, and time of collection, as well as the test requisition number. For random urine collections, a 7.0 mL aliquot in an acid-washed container is typically required. Labels should avoid abbreviations and ensure clarity. Proper labeling prevents mix-ups and delays in processing. Special instructions, such as storage conditions, should also be noted. Adhering to these standards ensures the integrity of the sample and supports reliable diagnostic outcomes. Correct labeling is essential for maintaining patient safety and efficient laboratory operations. Accurate identification of urine samples is critical for timely and accurate results.
Labeling Tissue Samples: Unique Considerations
Labeling tissue samples involves unique considerations to ensure accurate identification and processing. The manual emphasizes the use of permanent, waterproof markers to label containers, as tissues are often subjected to various treatments. Labels must include the patient’s name, medical record number, date, and specific anatomical site. For example, a biopsy sample from the liver must be clearly differentiated from one taken from the kidney. Additional information, such as the type of fixative used, may also be required. Proper labeling prevents cross-contamination and ensures that samples are correctly matched to patient records. Strict adherence to these guidelines is crucial for maintaining the integrity of tissue samples and supporting precise diagnostic outcomes. Special handling instructions, if applicable, should also be clearly indicated on the label to avoid processing errors. Accurate labeling is vital for patient safety and laboratory efficiency.
Troubleshooting Common Labeling Issues
Labeling tissue samples requires meticulous attention to detail due to their sensitive nature. The manual highlights the necessity of using permanent, waterproof markers to ensure labels remain legible through various laboratory processes. Each specimen container must be clearly marked with the patient’s name, medical record number, collection date, and specific anatomical location. For instance, a liver biopsy must be distinctly labeled from a kidney sample to prevent mix-ups. Additional details, such as the type of fixative used, may also be essential. Proper labeling ensures accurate identification, prevents cross-contamination, and maintains the integrity of the sample. Adhering to these guidelines is critical for reliable diagnostic outcomes and patient safety.
Identifying and Correcting Labeling Errors
Identifying and correcting labeling errors is crucial to ensure patient safety and accurate test results. Errors may include missing or illegible labels, mismatched patient names, or incorrect specimen types. The manual advises a systematic approach: first, verify all label details against the patient’s records and request form. Use permanent markers to prevent smudging, and ensure labels are affixed securely. If an error is detected, immediately void the incorrect label and replace it with a new one. Document the correction in the patient’s file to maintain transparency. Proper training and double-checking by a second person can minimize such mistakes. Timely correction prevents delays in diagnosis and treatment, ensuring reliable outcomes. Adhering to these protocols enhances overall laboratory efficiency and patient care quality.
Preventing Future Mistakes: Proactive Strategies
Preventing labeling errors requires a proactive approach to minimize risks and enhance accuracy. Implementing standardized labeling protocols ensures consistency across all specimens. Staff training is essential to familiarize personnel with manual guidelines and emphasize the importance of attention to detail. Regular audits of labeled samples can identify potential issues before they escalate. Additionally, incorporating technology, such as barcode scanning, can automate labeling processes and reduce human error. Establishing a double-check system, where a second person verifies labels, further enhances reliability. Continuous feedback loops allow for the refinement of protocols based on past errors. By fostering a culture of vigilance and accountability, healthcare facilities can significantly reduce labeling mistakes and improve patient care outcomes. These strategies collectively ensure accurate and reliable specimen identification, safeguarding diagnostic integrity.

Advanced Labeling Techniques
Advanced labeling techniques involve specialized methods for metabolic and anatomical studies, ensuring precise specimen identification. These strategies optimize efficiency and accuracy in complex laboratory settings, enhancing overall reliability.
Specialized Labeling for Metabolic Studies
Specialized labeling for metabolic studies involves precise specimen identification to track biochemical processes accurately. This method ensures consistency and prevents cross-contamination, critical for reliable data interpretation. Advanced techniques include time-stamped labeling and unique identifiers for longitudinal studies. The Labeling 2-2 Reference Manual provides detailed guidelines for handling metabolic samples, emphasizing accuracy and traceability. These strategies are vital for clinical and research applications, ensuring the integrity of metabolic studies and patient safety. By adhering to these protocols, healthcare professionals can confidently conduct complex analyses, advancing both diagnostic and therapeutic outcomes. Proper labeling in metabolic studies is indispensable for maintaining the highest standards of scientific rigor and patient care.

Labeling Strategies in Anatomical Studies
Labeling strategies in anatomical studies require meticulous attention to detail to ensure clear identification of structures. The Labeling 2-2 Reference Manual offers specific guidelines for anatomical labeling, emphasizing the use of standardized terminology and precise marker placement. These strategies enhance clarity in diagrams and specimens, aiding education and research. Advanced techniques include color-coding and hierarchical labeling to differentiate complex structures. The manual also addresses common errors, such as incomplete or illegible labels, providing corrective measures. Adherence to these protocols ensures consistency and accuracy, which are crucial for effective communication in anatomical studies. By following the manual’s recommendations, professionals can improve the quality of anatomical labeling, supporting both educational and clinical applications.
Case Studies and Real-World Examples
The Labeling 2-2 Reference Manual has been successfully implemented in healthcare facilities, reducing specimen labeling errors and improving patient safety through standardized protocols and clear guidelines.
Successful Implementation of Labeling Protocols
Case studies highlight the effectiveness of the Labeling 2-2 Reference Manual in real-world healthcare settings. Hospitals and labs have reported significant reductions in specimen labeling errors after adopting the manual’s guidelines. For instance, one medical facility implemented the manual’s protocols for blood and urine samples, resulting in a 30% decrease in mislabeled specimens. This success was attributed to the manual’s clear instructions and standardized labeling procedures. Additionally, the manual’s emphasis on training and quality control measures ensured sustained compliance. These examples demonstrate how the Labeling 2-2 Reference Manual can be effectively integrated into routine practices to enhance patient safety and operational efficiency.
Lessons Learned from Labeling Challenges
Challenges in specimen labeling have underscored the importance of adherence to the Labeling 2-2 Reference Manual. Common issues include missing patient identifiers and illegible handwriting, which can lead to specimen mix-ups. Lessons learned emphasize the need for staff training and regular audits to ensure compliance. For instance, one lab reported that implementing double-checking procedures reduced labeling errors by 25%. Additionally, the use of automated labeling systems has been identified as a critical solution to minimize human error. These experiences highlight the importance of combining clear protocols with technological advancements to achieve accurate and reliable labeling practices in healthcare settings.
Future Trends in Labeling
Emerging technologies like automated labeling systems and advanced tracking software are transforming specimen identification. Integration of AI for error reduction and sustainable labeling practices are expected to dominate future trends.
Emerging Technologies in Labeling
Emerging technologies are revolutionizing the labeling process, enhancing accuracy and efficiency. Barcode systems and RFID tags are being widely adopted to minimize manual errors. Automated labeling machines, capable of printing and applying labels in real-time, are gaining popularity. Additionally, AI-driven algorithms are being integrated to detect and correct labeling discrepancies. These advancements ensure compliance with regulatory standards and improve traceability. For instance, the BISMUTH, URINE RANDOM test requires precise labeling, which can be achieved through these technologies. The use of digital tools also enables real-time tracking of specimens, reducing delays in diagnostic processes. As these technologies evolve, they promise to streamline labeling workflows, ensuring safer and more reliable specimen identification across healthcare settings.
Evolution of Labeling Standards
Labeling standards have undergone significant transformations to meet the growing demands of healthcare accuracy and patient safety. Historically, labeling relied on manual processes, which were prone to human error. Over time, standardized protocols were developed to ensure consistency across laboratories and medical facilities. Today, these standards are regularly updated to incorporate advancements in technology and regulatory requirements. For instance, the transition from handwritten labels to barcode systems has significantly reduced errors. Additionally, the integration of digital labeling tools has enhanced traceability and compliance with global healthcare regulations. These evolving standards are critical for maintaining the integrity of specimens like the BISMUTH, URINE RANDOM test, ensuring accurate results and reliable patient care. Continuous updates to labeling standards are essential for adapting to future challenges in healthcare diagnostics.
The Labeling 2-2 Reference Manual is a vital resource for ensuring accurate and consistent specimen labeling. By adhering to its guidelines, healthcare professionals can enhance patient safety and diagnostic accuracy, fostering trust and reliability in laboratory practices.
The Labeling 2-2 Reference Manual emphasizes the importance of accurate specimen labeling in healthcare settings. It outlines specific guidelines for blood, urine, and tissue samples, ensuring consistency and reducing errors. The manual highlights the consequences of mislabeling, such as delayed diagnoses or incorrect treatments. Key procedures include using permanent markers, avoiding abbreviations, and verifying patient identifiers. Best practices encourage double-checking labels before testing and documenting corrections. The manual also addresses troubleshooting common labeling errors, such as smudged or incomplete labels. By adhering to these standards, healthcare professionals can enhance patient safety and maintain reliable laboratory results. This resource is invaluable for training and ensuring compliance with regulatory requirements.
Final Thoughts on Effective Labeling Practices
Effective labeling practices are critical for ensuring patient safety, accurate test results, and operational efficiency in healthcare settings. The Labeling 2-2 Reference Manual underscores the importance of consistency, clarity, and adherence to established protocols. By using permanent markers, avoiding abbreviations, and verifying patient identifiers, healthcare professionals can minimize errors. Double-checking labels before processing and maintaining clear communication channels further enhance accuracy. Training staff regularly and implementing quality control measures are essential for sustaining high standards. Ultimately, precise labeling practices not only safeguard patient outcomes but also uphold the integrity of laboratory processes. Continuous improvement and adherence to guidelines ensure reliable results, making the Labeling 2-2 Reference Manual an indispensable resource for healthcare professionals.
